
Female sexual arousal disorder (FSIAD) occurs when your body isn’t responding to sexual stimulation. However, the experience can be different for each woman. While some women with FSIAD experience symptoms every time they try to engage in sexual activity, others may have more …

Female infertility refers to infertility whose root cause lies with the women. Infertility is a complex issue that can have many causes. Conception and pregnancy are very delicate and complicated processes that require the right conditions and timing in order to be successful, hence infertility will occur if the right conditions are not met.

If you’ve experienced weight loss with Ozempic or a similar weight-loss drug, you may be wondering if some other changes you’ve noticed could also be linked. Is there such a thing as Ozempic vagina? Explore the different ways in which Ozempic can affect your vaginal health and appearance.

Menopause can have a profound impact on sex drive and sexual health. For many women, desire and enjoyability nosedive leading up to, during, and after menopause. A lack of information regarding hormonal changes can leave women in the dark about their options. Quality, enjoyable sex after menopause is possible …

Changes to the genitalia are more common than most realize. Vaginal rejuvenation aims to address those concerns through repair and revitalization. While there are many surgical options available, surgery is not always necessary. There are several non-surgical vaginal rejuvenation treatments to provide life-changing results without …

Vaginoplasty procedures are more popular than ever. Thousands of women across the country elect to get this surgery for a variety of reasons. It’s a form of cosmetic surgery and reconstructive that can repair the pelvic floor and walls of the vagina. This procedure can help women address vaginal injuries after childbirth, tighten …

Skin darkening and general hyperpigmentation are relatively common issues that can arise due to sun exposure and age. Having a dark vaginal area usually isn’t a health concern. It’s normal for women of all complexions to experience darkening around the vulva and other intimate areas. However, the extent of the …
In addition to being uncomfortable, vaginal laxity is also anatomically unsettling. Many women experience tears and laxity during vaginal delivery. This is also known as looseness of the vagina. With the vaginal canal widening a considerable amount while in labor, the vagina usually does not return to its pre-childbirth state …….

Unfortunately, stigmas surrounding the discussion of issues like this force many to deal with the negative aspects of vaginal laxity in silence. But you don’t have to settle for undesired looseness. This problem is more common than most realize, affecting most women at some point in their lives. It’s not just a cosmetic issue. Laxity can negatively …

Lichen sclerosus is a non-STD inflammatory condition that can severely impact a woman’s quality of life. Once it develops, lichen sclerosus can cause itchy and painful patches of thin, wrinkled, and discolored skin to develop. The lichen sclerosus symptoms …

The vaginal canal can be of different shapes and sizes. In fact, it can change throughout the day. But when the vagina is shallower than normal, you can experience pain during intercourse, menstruation, and more. But what is a shallow vagina, and how do you know if you have one?

While some discomfort is normal, many women unknowingly have endometriosis. It can develop in women only a few years after the first menstrual period. The signs of endometriosis are easy to mistake for other conditions, and it’s common for women to mistake them for standard period pain ….

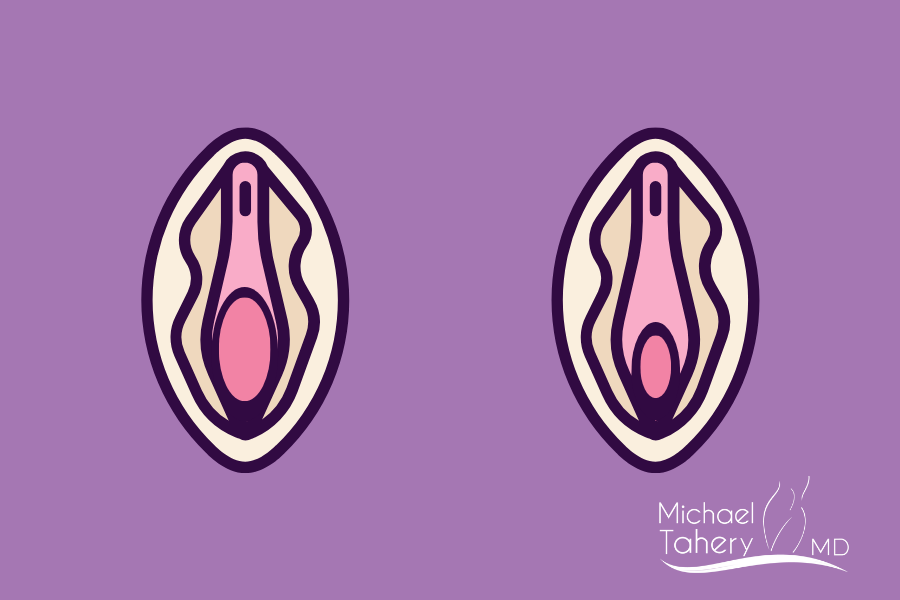
Traditional labiaplasty is an outpatient surgical procedure that involves making incisions to remove excess tissue. While surgical labiaplasty can provide impressive results, it’s not your only option. Non surgical labiaplasty can improve the size and overall appearance of the labia using lasers and radiofrequency devices …..

Like other cosmetic surgeries, labiaplasty can be life-changing, helping you feel comfortable in your body. But despite the good this procedure can do, many women are concerned about the potential pain and the recovery process. So, is labiaplasty painful? The good news is that labiaplasty is considered a relatively minor surgery. Usually under local anesthesia, allowing …

Will labiaplasty surgery get rid of camel toe? Is a common question among women who feel self-conscious about seeing the outline of their vaginal lips through their clothing. While we all understand that this is part of basic anatomy, a camel toe can still make it difficult to feel comfortable when wearing jeans, leggings, yoga pants …

Contrary to popular belief, fibroids don’t have to be massive to cause discomfort and affect your quality of life. There is no such thing as a size threshold that dictates when women should get small fibroids treatment. Whether or not you should seek treatment depends entirely on the symptoms they create. Fibroids of any size can cause pain and ….

While recovery times vary by patient, vaginoplasty full recovery typically takes six to eight weeks. However most patients return to normal activity within a few days. It’s common for patients to experience some swelling, tenderness, bruising, and soreness in the days and weeks following surgery. While discharge and ….

There’s no need to live with the debilitating consequences for sleep, sexual health, general happiness, and confidence created by vaginal atrophy also known as atrophic vaginitis. Vaginal Atrophy is largely caused by the natural reductions in estrogen experienced both during and after menopause.

Have you decided that it’s time for some rejuvenation? Vaginal rejuvenation is a restorative, confidence-boosting surgical and non surgical procedure that allows patients to address both physical discomfort and aesthetic concerns. Take a look at the factors that might influence vaginal rejuvenation cost in Los Angeles.

While testosterone is known as a male sex hormone and estrogen is a female sex hormone, everyone needs both to remain healthy. Women have testosterone as well, however only a fraction of what men do. Your body produces testosterone in many places. Testosterone in young women originates from the ovaries …

Hymen repair, also known as hymenorrhaphy, is a procedure that revolves around an often-misunderstood part of the female anatomy. Sometimes called the “virginity tissue,” the hymen is a band of tissue that sits at the opening of the vagina, and it’s often torn during intercourse, exercise, tampon insertion, and …

The labia can change over time. While many women feel prepared to deal with the menstrual changes that occur as they approach menopause, they are taken aback by changes in the appearance of the vagina. It’s not uncommon for the labia to experience changes in size, shape, and elasticity at different stages of life …

Sometimes referred to as “the great change of life,” menopause is a natural part of the aging process for women. It marks the end of a woman’s reproductive life, and with that end comes significant changes. Its symptoms last several years and changes begin much earlier than most realize and its ….

Vaginal rejuvenation is an umbrella term used to describe several unique procedures. The vagina is a complex organ and will continue to change through puberty, pregnancy, and menopause. As you age, the vagina can experience several issues. Investing in a vaginal rejuvenation procedure is a ..

Extreme weight loss is no easy feat, and it deserves all the praise in the world. Taking charge of your body and health is nothing short of inspirational, and you’re likely reaping the rewards of your hard work every day. Your weight loss journey can positively ..

Genital bleaching in Los Angeles is a standard cosmetic procedure that’s become increasingly popular in recent years. Yet, it’s a treatment that few women talk about openly. It’s more prevalent than most people realize, but the ongoing stigma of sexual health and intimate procedures leaves a lot to the imagination.

Also known as MI vaginoplasty is the surgical repair of the pelvic floor and vaginal walls that can be performed under local anesthesia and was designed and created by Dr. Tahery. It’s a versatile procedure that targets your unique needs. Many women choose to combine it with other surgeries like labiaplasty.

One crucial detail that makes fibroids affect pregnancy and fertility is location. These tumors can develop in various parts of the uterus. Submucosal fibroids generally have the most impact on fertility. These growths appear just under the endometrium and protrude into the uterine cavity. This type of fibroid …

Pelvic organ prolapse is a particularly troublesome issue that can lead to incontinence, uncomfortable pelvic pressure, and a host of other problematic symptoms. Pelvic reconstructive surgery aims to repair those abnormalities, helping women reclaim their bodies and confidence.

Thanks to the growing popularity of vaginal rejuvenation services, more and more women are turning to procedures like clitoral hood reduction surgery to reclaim their sexual health and confidence. Also known as a Hoodectomy, this procedure can address several concerns. Its main goal is to …

Urinary tract infections, also known as UTIs, are a common problem among women. Researchers believe that more than half of all women will experience a UTI at some point in their life. A woman’s urethra is much shorter than a man’s, leading to more opportunities for bacteria ….

One of the most common concerns regarding labiaplasty is its effects on pregnancy and giving birth. Is it better to get a labiaplasty before or after pregnancy? The right choice for you depends entirely on your needs and goals. Interest in labiaplasty timing is reasonable considering how it ….

70 percent of women are diagnosed with fibroids during their reproductive years. The non-cancerous growths are so common that the average woman typically has six to eight without even knowing. While a vast majority of fibroids are benign, many still require treatment ….

Coverage can vary based on the details of your policy and your condition. Like other procedures that tiptoe the line between cosmetic and medically necessary, Labiaplasty coverage also depends on the reasons for getting it. For most women, the cosmetic reasons for Labiaplasty are the biggest draw …
Women with vaginal looseness are likely experiencing other issues. It’s not a product of too much penetrative sex. The good news is that there are several ways to address tightness concerns. Vaginal tightening encompasses surgical procedures, laser treatments, and more. Tightening can improve elasticity to …..

Most women are familiar with menopause and all the changes that come with it. However, few understand what happens in the years leading up to it. Perimenopause is a transitional phase that occurs before the ovaries officially stop releasing eggs …

Labial hypertrophy is a common condition that refers to the size of the labia or vaginal lips. It’s a term that describes noticeable vaginal asymmetry. While the labia aren’t perfectly symmetrical in most women, hypertrophy is when one or both lips are more prominent than usual. This form of hypertrophy is usually not a serious …

Your menstrual cycle provides tons of information about your overall health. Irregular periods are not something you should ignore.
A standard menstrual cycle can range from 21 to 35 days. Meanwhile, the period itself lasts four to seven ….
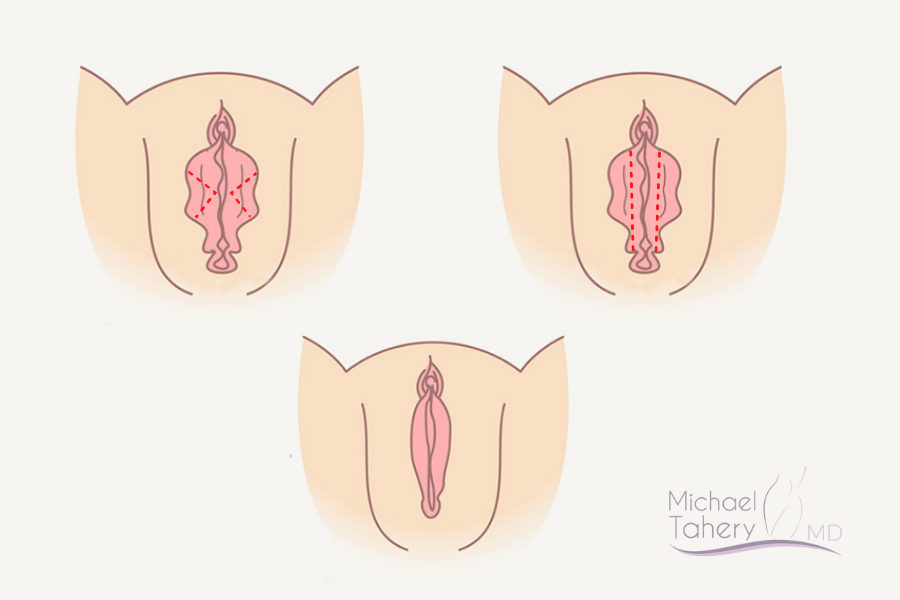
Deciding to undergo a labiaplasty procedure is a big step in gaining confidence and sexual empowerment. Labiaplasty is one of the fastest-growing cosmetics surgeries in Los Angeles because it can have a significant impact on the overall appearance of the vagina. All the while, it may address discomfort and improve your …..

Even though results are seen immediately after the labiaplasty surgery, full healing and final result take time. Like any other surgical procedure, women will require some downtime to recover after a labiaplasty. The recovery process will vary from woman to woman. However, most will follow a basic timeline after surgery.

In the majority of cases, labiaplasty is done to alter the shape of the labia as per patient’s desires or correct significant discrepancies in size and shape between the two lips. It is also done to remove the darkened portions of the labia or to repair a delivery scar. Then there are cases where the …..

Urinary incontinence in women is a common medical condition and many are too embarrassed or shy to talk about. Despite the stigma, loss of bladder control plagues women of all ages. It’s most often associated with old age and post parting, but other health complications can also ……

Our skin gets wrinkled when we age or when we lose weight. Also as hormonal changes occur as in menopause, it affects the connective tissues supporting our skin. Unfortunately it’s a fact of life that we can not avoid. Exercise helps tighten the muscles, hydration helps avoid dryness ……

Labiaplasty is a potentially life-changing procedure that helps women feel more confident in their skin. Like other cosmetic procedures, it aims to improve aesthetics safely. It involves changing the physical appearance …..

A pelvic floor disorder has the potential to disrupt your life in many ways. The pelvic floor is a series of muscles and connective tissue that runs from the pubic bone to the bottom of the spine or the coccyx. It acts as a sling to support crucial organs like the bladder, bowels, and uterus. Furthermore, the contracting and relaxation of these muscles …

While once a taboo topic, women’s sexual health is more widespread than ever. Many procedures exist to improve a woman’s self-esteem and libido. From vaginal tightening to full vaginal rejuvenation, these treatments allow women to take the reins on their sexual health and experience positive change. One treatment that’s growing in ……..

Endometriosis diet aims to minimize foods that boost estrogen levels or certain types of prostaglandins, which can contribute to endometriosis flare-ups, pain, and other complications from the disorder. Consuming the right foods can help to soothe symptoms and reduce inflammation ……..

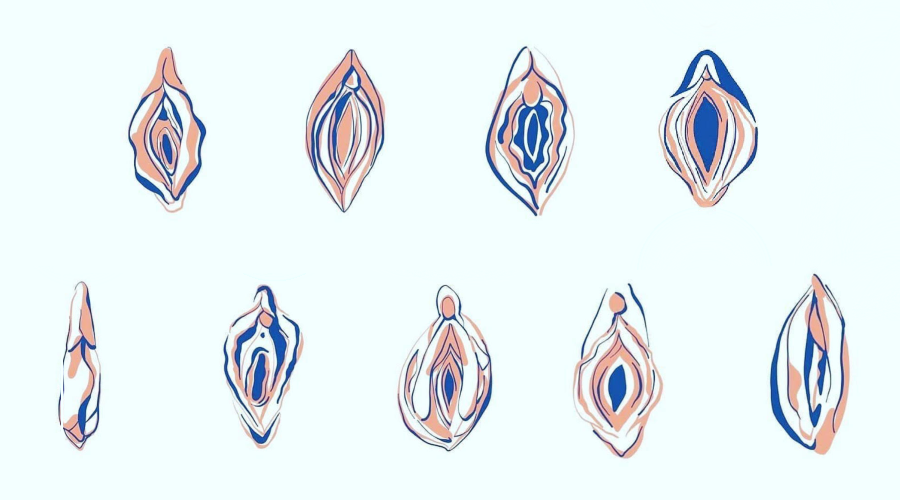
Sex education, while important, often excludes talk of the female body. More specifically, the shape, size, and elasticity of a woman’s vagina. Unfortunately, this leads many women to be confused about what’s normal. Women have also long been discouraged from talking about their genitalia. This gives room for rumors to dominate …

The arrival of a new baby is nothing short of a miracle. While the transition into motherhood can be overwhelmingly exciting, it can also wreak serious havoc on the female body. Though not every woman experiences significant physical changes, the majority of new moms undergo their fair share of body alterations. More often …..

Whether you prefer to catch some Z’s or hit the hay, sleep plays a prominent role in our well-being. In addition to helping us recharge, sleep also allows us to retain information that we’ve acquired throughout the day. With a good night’s rest, you can also synthesize hormones, grow muscle …..

Hormone replacement therapy (HRT) is a treatment used in women to reduce the symptoms associated with menopause. From the first menstrual period up to menopause, healthy ovaries (including the pituitary gland) regulate female hormones – estrogen and progesterone as well as male hormone production ….

Births, physical injuries, tissue loss and even physiological aging are the most common reasons why women undergo aesthetic procedures performed in the perineum, i.e. the area located between the vagina and the anus. The reason is both the desire to change the appearance of the skin and the opening but also to improve the quality of life and sexual ….
“Experts estimate that a uterine condition called adenomyosis may affect between 20% to 35% of women. The condition can cause painfu, heavy, prolonged”
“Like heartburn and cankles, expectant moms are more prone to this itching, burning condition. Here’s what you need to know about diagnosis, treatment and”
“It can be difficult to have conversations about sexually transmitted infections like HIV, herpes, and genital warts with one partner, but thanks to stigma around STIs, having conversations with multiple partners increases”…
Hormonal changes impact your nether regions in many frustrating ways besides vaginal dryness. About half of all menopausal women experience more itching, burning and irritation down below than they did during their fertile years—as well as a greater

Vaginal Rejuvenation and Labiaplasty are surgical and laser procedures that women usually opt for after they have given birth, gone through some hormonal changes or as they age and experience weakened vaginal muscles, change

There are numerous hormones in a woman’s body influencing fertility. The mere presence of these hormones are not sufficient. These hormones need to be available in sufficient amounts and work in a balanced manner in order to achieve ovulation. The following is

Pelvic Pain is pain that is felt in the lower part of the abdomen where the bladder, bowels, uterus, and ovaries are located. This kind of pain usually stems from the reproductive system, urinary system or the digestive system and can be classified as either chronic or acute pain. There are a number of
Uterine fibroids are noncancerous tumors that grow in the muscle or wall of the uterus and usually only require treatment when symptoms such as heavy bleeding, pain, infertility, and frequent urination becomes a problem. There are various ways of treating fibroids
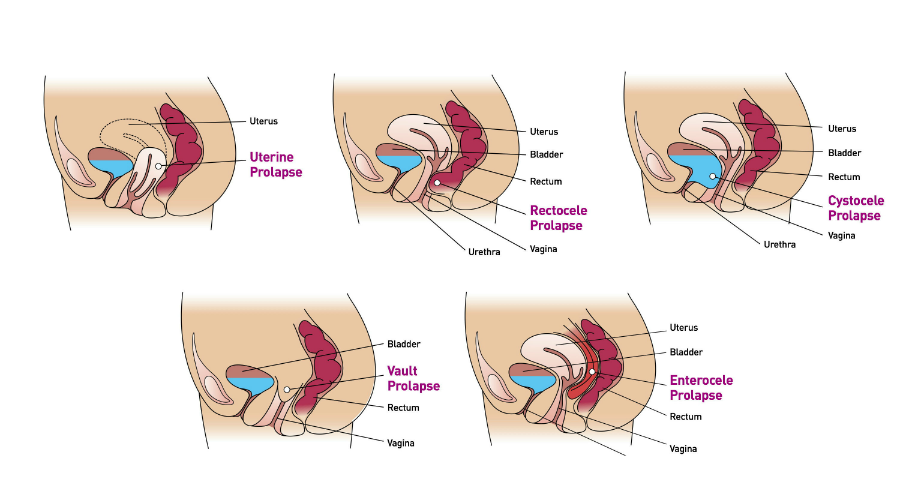
Most women after a vaginal delivery experience some trauma and damage to the supportive structure of their vagina. These supportive structures are scaffolding that maintains the position and the proper functioning of the organs surrounding the vagina

Women are at increased risk of depression during perimenopausal transition due to hormonal changes in this period so close to menopause. This syndrome is called perimenopausal depressive disorder or PMDD. Researchers hypothesis that during

Nonsteroidal anti inflammatory drugs, also known as NSAIDS, are the most commonly used over the counter pain medications. They are marketed under brand names such as aspirin, ibuprofen,advil, aleve and many others.

Period pains or the menstrual cramps are the most common complaint in menstruating women of all ages. Studies show 60-70% of women complain of cramps and 13-33% of women suffer from severe cramps. These symptoms can be so severe and disruptive that 24-34% of women fail to report for

Vaginal infections are one of the most common conditions women complain about. They present as abnormal odor, itching, and discharge. They show up as recurrent urinary tract infections, pain with intercourse, and persistent and chronic irritations inside and outside of the vagina.

Endometriosis is the implantation of the endometrial tissue in the pelvis or the abdomen. Endometrial tissue is what you see on your pad during menses. We think it finds its way to the inside of the abdomen through the fallopian tubes, tubes attaching the inside of the uterus to the inside of the abdomen. In most

“Can i still get pregnant?” “how much longer do i have? Time goes by fast. While we are going to school, building a career, and getting ready to get pregnant, time slips away. The number of women trying to get pregnancy after the age of 35 is growing. At 35 the chance of getting pregnant is 29% in each cycle, almost half of that before …..

“Do i need hormones?” “Are all hormones the same?” “what is the safest and the best hormones and when should i start?”These are the most common questions I am asked from women transitioning through perimenopause or in menopause. Women concerned about changes they see in themselves, friends …
“I can’t lose weight, my face is full of acne and thick hair, and my periods are very irregular. What is going on with my body?” These are some of the most common signs of a very common hormonal condition called polycystic ovarian syndrome or (PCOS). 10-15% of women …….

Hormonal imbalance occurs when there are either too little or too much hormones in the body. Even though we might not get to see or feel the hormones, they play a very important role in the functioning of the organs and the body as a whole, hence even the slightest hormone

“Mothers are the root of the family tree. Without a healthy root the tree will wither. Self care is non-negotiable, it’s survival.” Postpartum mood disorders range from short lived “blues” (80% of new mothers), to more severe depression (20%), and much less common psychosis (1/1000). Causes are complex and treatment may require

‘Menopause-related cognitive impairment happens to women in their 40s and 50s, women in the prime of life who suddenly have the rug pulled out from under them,’ an expert says. Dr. Gayatri Devi’s patient, a 55-year-old former headmistress,
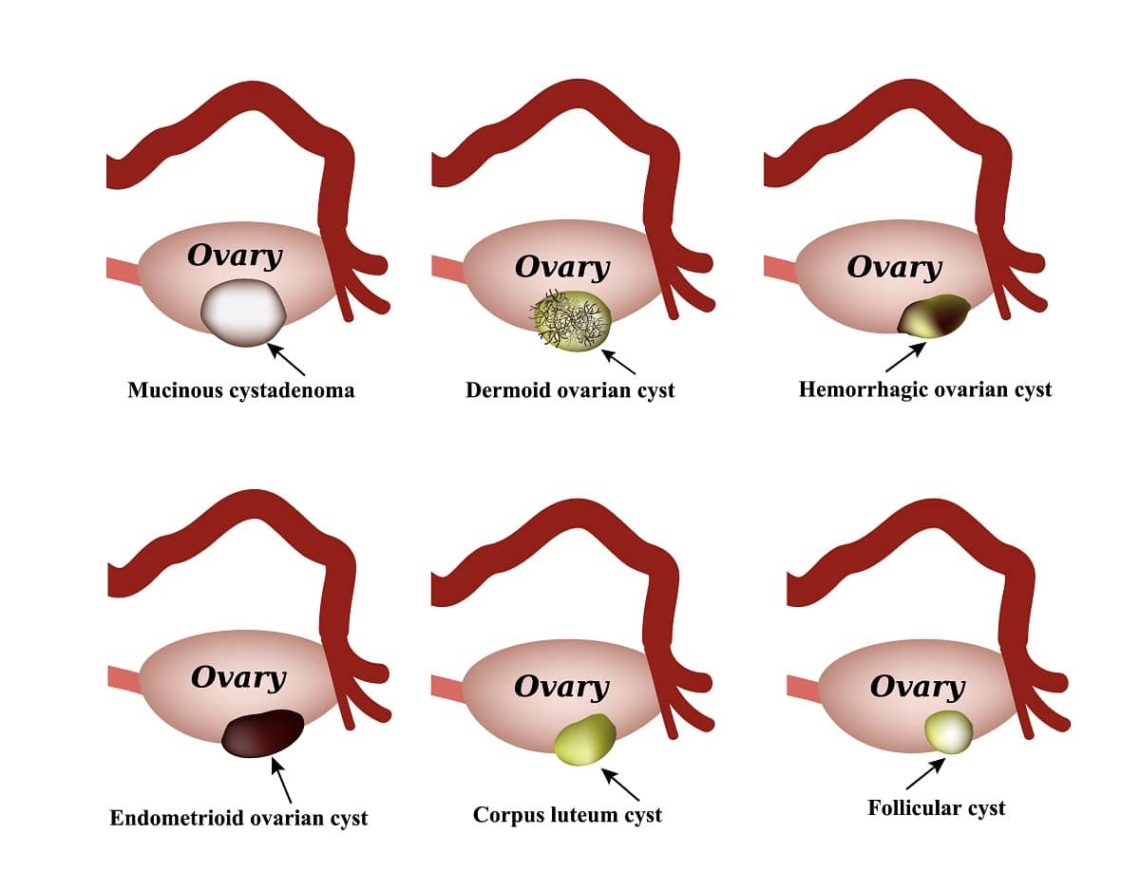
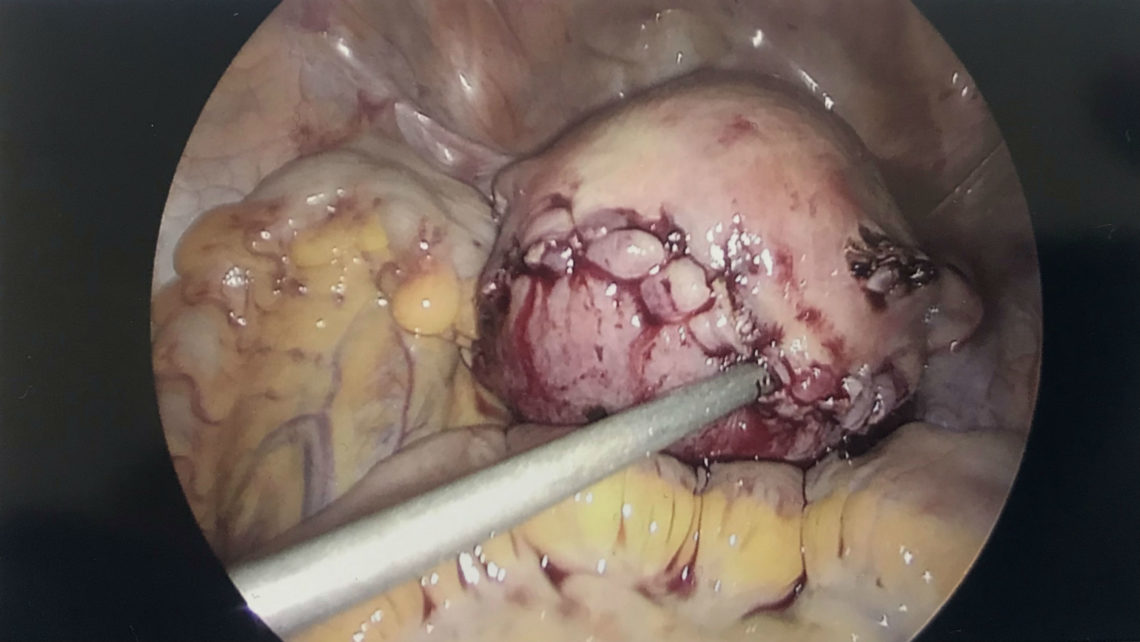
Ovarian cysts are one of the most common findings in women of reproductive age. The majority of women I see in the office with ovarian cysts complain of a combination of menstrual irregularities, pain with menstruation or intercourse, and abdominal distention. In some cases, the pain and bleeding is so severe

On any given day in my practice, I am faced with the seemingly straight forward, yet complex question from women at various stages of their lives; “can I get pregnant?”. Women in their twenties and nervous about their health; those in their thirties worried about the metaphorical clock ticking away; and women in their forties

Frequently, I hear a variation of this sentence from mothers very soon after childbirth. Too frequently, if you ask me.It is the symptom of our fastpaced life. We have no time to waste on recovery. We hear, “Be strong. Get back to work. All mothers do it.” Work, family, child, and pretty much anyone else comes first. No matter what a mother

Hemorrhoids are painful varicose veins in the anal area, which can get inflamed and cause significant pain and discomfort. Traditional surgical treatment involves excision of the hemorrhoids that can be very painful with a long recovery time. Using radiofrequency and electrocautery, we are able to treat

Postpartum urinary incontinence is a common condition many women face post pregnancy. Pregnancy and a vaginal delivery can cause increased pressure on the nerves that control the bladder (less common after a c-section delivery) and may result in a higher frequency of urination and urgency.

Yes, you read correctly. Recent studies show multivitamin use in healthy people not only decreases healthiness but also increases the risk of death. The exact conclusion from one study is as follows: “Most supplements do not prevent chronic disease or death,
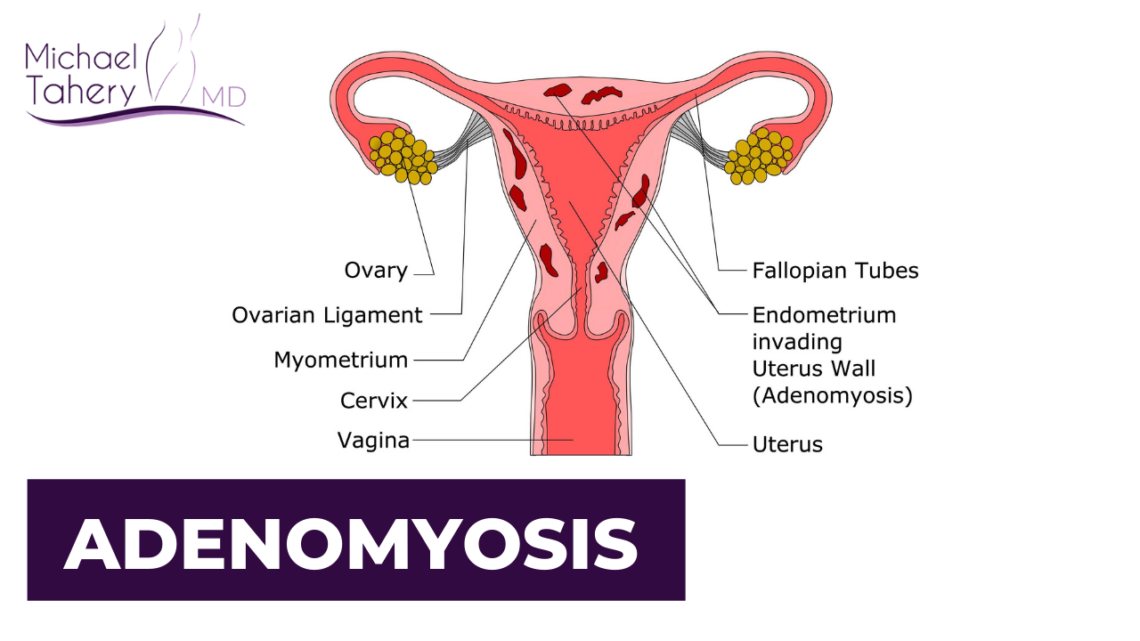
One of the most common conditions women complain of is heavy vaginal bleeding and pain during their menstruation cycle. Adenomyosis, or uterine endometriosis, is one of the most prevalent conditions

As the baby grows, so does the uterus carrying the baby. This growth stretches the skin over the enlarging uterus. Stretch marks are the red and brown streaks which eventually turn white, and sometimes itchy, that appear on or around your belly. They are a ……

As the level of estrogen in women decreases in perimenopause and menopause, shrinkage and dryness of the vaginal and urinary organs occur. The tissues thin out and the blood flow to the genitalia decreases. These changes can …..

I hear this so frequently in my office. Cyclic changes in mood and physical discomfort that usually starts after ovulation and ends with a period is called premenstrual syndrome and is often referred to as PMS. Feelings of depression, anxiety, nervous agitation, breast tenderness, and cravings are …
Interstitial cystitis (IC) is a chronic pelvic pain condition that has its origin in the bladder. Two to seven percent or the population (primarily women) suffer from this potentially debilitating condition. Women with recurrent urinary tract infection symptoms and negative cultures …..

Fourth trimester is the three month period after delivery when a mother’s body deals with the residual changes from carrying the pregnancy and child birth. This time period is critical since neglect in correcting these changes can lead to chronic lifelong issues. ……

One of the most common conditions in women is endometriosis. It occurs in 1 out of 10 women. The symptoms are usually persistent pain with menstruation, bloody cysts of the ovary and fertility issues. It is usually considered to be a benign condition. However, for years there has been ……

Adrenal fatigue is one of the most common hormonal abnormalities in our society. The day to day stress from work, family and society, added to the changes that we and nature inflict on our bodies causes the overproduction and eventual depletion of cortisol, an adrenal hormone. The overuse and …….

Anna had stopped by my office today for a six month follow up. Anna is a 25 year old woman who complained of chronic pain with sex a year ago. Anna lives in Texas and had come to see me because she did not feel that the physicians she had seen for this problem in Texas were able to help her with her……..

Now, one more reason to consider weight loss. A recent study shows that women who are overweight, and continue to gain weight, have intercourse less frequently and a significantly decreased desire for sex. This has been attributed to possible changes in hormonal patterns,

You are dieting, exercising regularly, doing your best to stay healthy and fit and lose some weight but it’s not working. Why you ask? It may be the toxins in your food and environment that you are exposed to that are working against you. Biphenol A is a known and banned toxin that has been used in ….

Anna had stopped by my office today for a six month follow up. Anna is a 25 year old woman who complained of chronic pain with sex a year ago. Anna lives in Texas and had come to see me because she did not feel that the physicians she had seen for this problem in …..

“Did you know we can put in a pacemaker for your bladder?”, I asked my 55 year old patient with chronic urinary incontinence. “A pacemaker for my bladder?”, she replied in disbelief.Many are surprised to hear what we do to help women control their urinary …

Testosterone is an essential hormone in a woman’s body. It is commonly known as a male hormone because men need a higher level of testosterone in their bodies. It peaks in women at the age of 20 and declines in perimenopausal years. They drop to their lowest levels during ……

Changes in estrogen and progesterone levels during the cycles may cause headaches in some women complaining of pain prior and during the menstrual cycles. Prior and during the menstrual cycle these hormone levels drop and are at the lowest levels . These headaches …….

Many women on hormonal contraceptives complain of decreased sex drive and vaginal dryness. In fact a recent study shows that 1 in 5 women reported lack of interest in sex after 6 months on the contraceptives. Hormonal birth controls such as pills, ……..